Sign up to receive the Institute on Aging newsletter
National Immunization Awareness Month for Older Adults
September 03, 2025

Fall Prevention Day: Protecting Independence, One Step at a Time
September 03, 2025
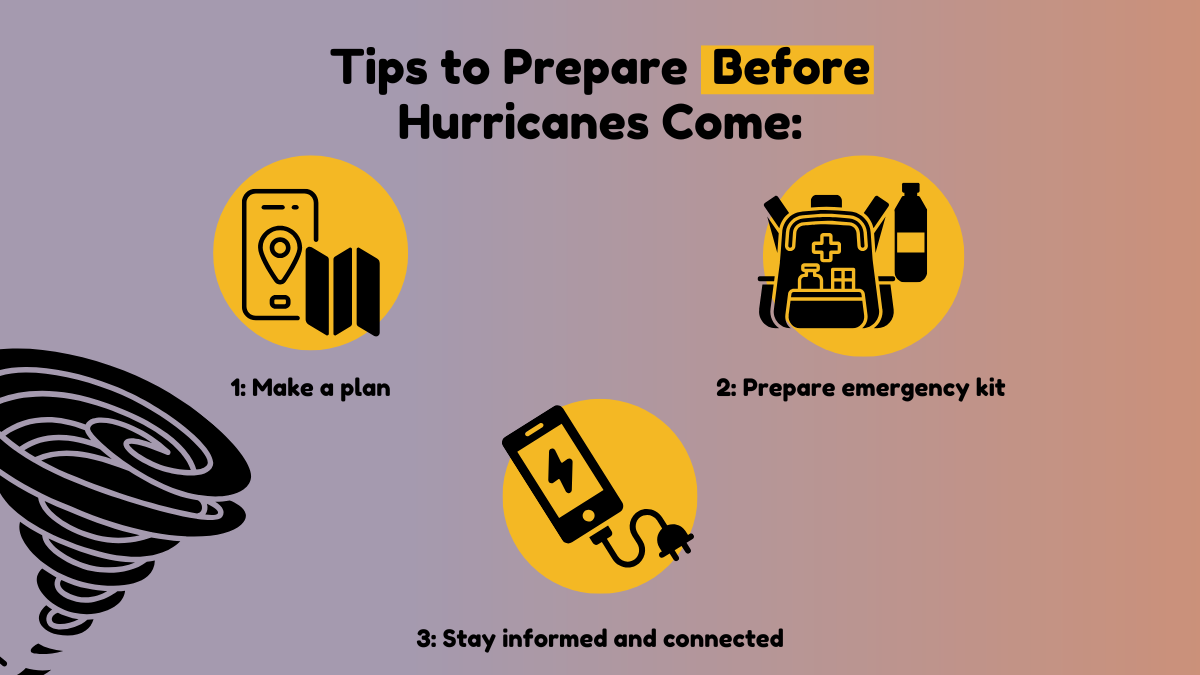
Tips to Prepare Before Hurricanes Come
June 24, 2025
Protecting Older Adults from Abuse
June 13, 2025

A heartwarming success: Walk to End Alzheimer’s
November 25, 2024

UTHealth Houston Hosted the 7th Annual Symposium on Aging Research
November 01, 2024

Roybal grant funds elder mistreatment research center
August 07, 2024

In Memory of Reverend William A. Lawson
May 21, 2024

In Memory of W. Andrew Achenbaum Jr.
May 10, 2024




.jpg)

.jpg)