At UTHealth Houston’s Pediatric Stroke Program, we provide clinical care and conduct research related to pediatric stroke and cerebrovascular diseases. Pediatric stroke is an underrecognized medical emergency, among the top 10 causes of morbidity and morality in the pediatric population. Currently, there is a shortage of pediatric neurologist specifically trained in diagnosis, acute management and long-term care of pediatric patients with cerebrovascular diseases. Our pediatric stroke program works closely with our partners at Children's Memorial Hermann Hospital to provide comprehensive medical care to children and families affected by pediatric stroke and cerebrovascular diseases.
Mission Statement
Our mission is to provide pediatric stroke patients with compassionate, comprehensive, and personalized care. We strive to support our patients by creating a nurturing and inclusive community for children with cerebrovascular disease. We are committed to performing innovative, cutting-edge research to continuously advance stroke care for young stroke survivors.

Pediatrics

UTHealth Houston Institute for Stroke and Cerebrovascular Diseases
.png)
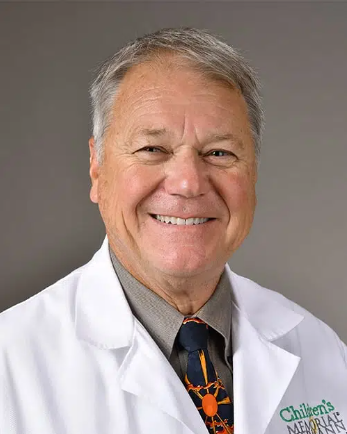
Director, Program for Pediatric Stroke and Cerebrovascular Disease at the Institute for Stroke and Cerebrovascular Disease at UTHealth Houston

Pediatric Stroke Clinic
The Pediatric Stroke Clinic with UT Physicians provides comprehensive stroke care for neonates, infants, children, and adolescents, who suffer from stroke or other cerebrovascular disorders, including moyamoya disease, intracerebral hemorrhage, neonatal stroke, and childhood stroke.
Though more common in adults, stroke is among the top 10 causes of death in pediatric patients, with few centers specializing in the treatment of pediatric stroke. We recognize these patients have specific and unique biologic and developmental needs, so we created a team of pediatric neurologists, vascular neurologists, pediatric neurosurgeons, nurses, and medical assistants. In coordination with our colleagues in hematology, oncology, pediatrics, and PM&R, we offer full-service coordinated care for any child who has suffered from cerebrovascular disease.
Pediatric Stroke Clinic is held weekly.
Clinic information:
Pediatric Stroke Clinic
6410 Fannin, 5th floor, Suite 500
Houston, TX 77030
Wednesday afternoons, 1pm-5pm
Appointments/Referrals:
Office Number: 713-500-7164
Email: [email protected]
Our Team:
Stuart M. Fraser, MD, Director
Melika Abrahams, RN, BSN
Pediatric Research
UTHealth Stroke Program has been conducting high caliber research in stroke for a long time, and our Pediatric Stroke Program is proudly carrying that tradition forward. We are part of the International Pediatric Stroke Study, where we work with other scientists from all over the world. We are also involved in other research studies funded by the National Institutes of Health, as well as conducting retrospective and prospective studies. These studies focus on how we can better treat stroke when it happens and help children recover afterwards.
Want to help us on this journey? We're always looking for volunteers to join our studies. Check out the information below to learn more about our studies that are currently recruiting participants. Together, we can make life better for kids with stroke.
-
I-ACQUIRE
Perinatal Arterial Stroke: A Multi-site RCT of Intensive Infant Rehabilitation (I-AQUIRE)
The UTHealth Pediatric Stroke Program is part of a nation-wide research study named I-ACQUIRE. This study is focused on helping young children who had a stroke when they were born. Specifically, we are trying to help children who had what is called a Perinatal Arterial Ischemic Stroke (PAS). Children who have difficulty moving one side of the body or the other from this type of stroke are potentially candidates.
In this study, we're testing two different levels of a new kind of therapy (I-ACQUIRE) to see how it helps kids aged 8 to 36 months who had PAS. This study will include 240 children, randomly divided into three groups:
- Moderate Dose group: Children in this group will receive the I-ACQUIRE therapy for 3 hours a day, 5 days a week, for 4 weeks.
- High Dose group: Children in this group will receive the I-ACQUIRE therapy for 6 hours a day, 5 days a week, for 4 weeks.
- Usual and Customary group: Children in this group will continue to receive their regular therapy in their community.
We will carefully track each child's progress from the beginning of the therapy, at the end of 4 weeks, and then 6 months after the therapy. Our goal is to learn more about the best ways to help children who have had a PAS.
To see study flyer CLICK HERE
The study is recruiting patients currently. If you are interested in having your child participate in this study or just want more information, feel free to reach out to Samantha Acosta at the email below.
PI: Stuart Fraser, MD
Coordinator: Maria Poblete
Contact: [email protected]
-
FOCAS
The FOCAS study is a critical research project being shared by multiple children’s hospitals in the United States aimed at improving treatment for children who may have a condition called Focal Cerebral Arteriopathy of childhood (FCA). FCA is a disease that can lead to stroke in children when one side of the brain does not receive sufficient blood supply.
While FCA is not common, it poses a serious risk due to its potential to quickly worsen, causing recurrent or expanding strokes. This study, FOCAS, is designed to determine the most effective treatment strategy.
The study will involve two groups:
Group A: Children in this group will receive a medication known as corticosteroids immediately upon suspicion of FCA.
Group B: Children in this group will receive corticosteroids only if their FCA shows signs of progression.
To gauge the effectiveness of the treatment, we will use a measure called the FCA Severity Score (FCASS). We will compare the score from the beginning of the study to 1 month later. In addition, we will measure the size of any strokes and assess overall child health outcomes at 6 months.
The FOCAS study is poised to significantly enhance our understanding and treatment of children with FCA. The study is expected to begin in September 2023.
The study is recruiting patients currently. If you are interested in having your child participate in this study or just want more information, feel free to reach out to Neena Patel at the email below.
PI: Stuart Fraser, MD
Coordinator: Antoinette W. Bernal-Tent
Contact: [email protected]
-
TOPSS
TOlerability of transcranial direct current stimulation in Pediatric Stroke Survivors
The TOPSS Study is a research project by the UTHealth Pediatric Stroke Program that's looking at new ways to help kids get better after a stroke. This study is for kids and teenagers who had a stroke when they were at least 1 month old and now have a hard time moving one side of their body.
In this study, kids will try a new type of treatment for stroke. They'll get regular occupational therapy, which helps them learn to do daily tasks, along with a special treatment called non-invasive neuromodulation, which uses safe and gentle electricity to try to help the brain recover. Kids between 5 and 19 years old who have trouble moving their arm because of a stroke can join this study.
If your child joins the study, they'll have 5 occupational therapy sessions to try to improve the use of their weak arm, and at the same time they'll also receive the non-invasive neuromodulation treatment. We hope that this might help them use their arm better after having a stroke.
Dr. Stuart Fraser is in charge of the study, and Melika Abrahams is the research nurse who will help with the study.
The study is open now and we are recruiting. If you or your child would like to be part of the study, you can email [email protected] or call Melika at 713-500-7164.
To see study flyer CLICK HERE
This study is partially funded through the Society of Vascular and Interventional Neurology Pilot Grant Program.
-
IPSS
The International Pediatric Stroke Study (IPSS) is the largest childhood stroke registry in the world. UTHealth and Children’s Memorial Hermann are part of this registry, joining a worldwide network of children’s hospitals who share data about pediatric stroke to learn important information to try to help children with stroke.
Dr. Stuart Fraser is the IPSS leader at UTHealth.
For more information, please visit the IPSS website:
UTHealth Houston Pediatrics
The mission of the Department of Pediatrics is three-fold:
- To provide the highest quality and cost-efficient medical care to infants, children, and adolescents entrusted to us
- To advance knowledge in biomedical, clinical, and behavioral science through our research programs
- To provide excellence and innovation in training the next generation of pediatricians and sub-specialists through our medical student, residency, and fellowship programs
Learn more about UTHealth Houston Pediatrics
Pediatric Stroke Publications
- A National, Electronic Health Record-Based Study of Perinatal Hemorrhagic and Ischemic Stroke
- Stroke In The Young
- Consensus-Based Evaluation of Outcome Measures in Pediatric Stroke Care: A Toolkit.
- International Prevalence and Mechanisms of SARS-CoV-2 in Childhood Arterial Ischemic Stroke During the COVID-19 Pandemic
- Association of De Novo RNF213 Variants With Childhood Onset Moyamoya Disease and Diffuse Occlusive Vasculopathy