Symptoms came and went at first—discomfort, incontinence, anxiety— until they became a part of her daily life, affecting her ability to play golf and be intimate with her husband. Yet it took three years after the first signs before Kim Cole, NP, sought treatment for what turned out to be a prolapsed bladder. The muscles supporting the bladder had weakened, causing her bladder to, as Kim puts it, try to fall out of her body.
“I was kind of in denial. I thought, ‘This will go away eventually,’ so I just let it be,” explains Kim. “But it was always there. I could feel it was always there. And I had to go to the bathroom frequently.”
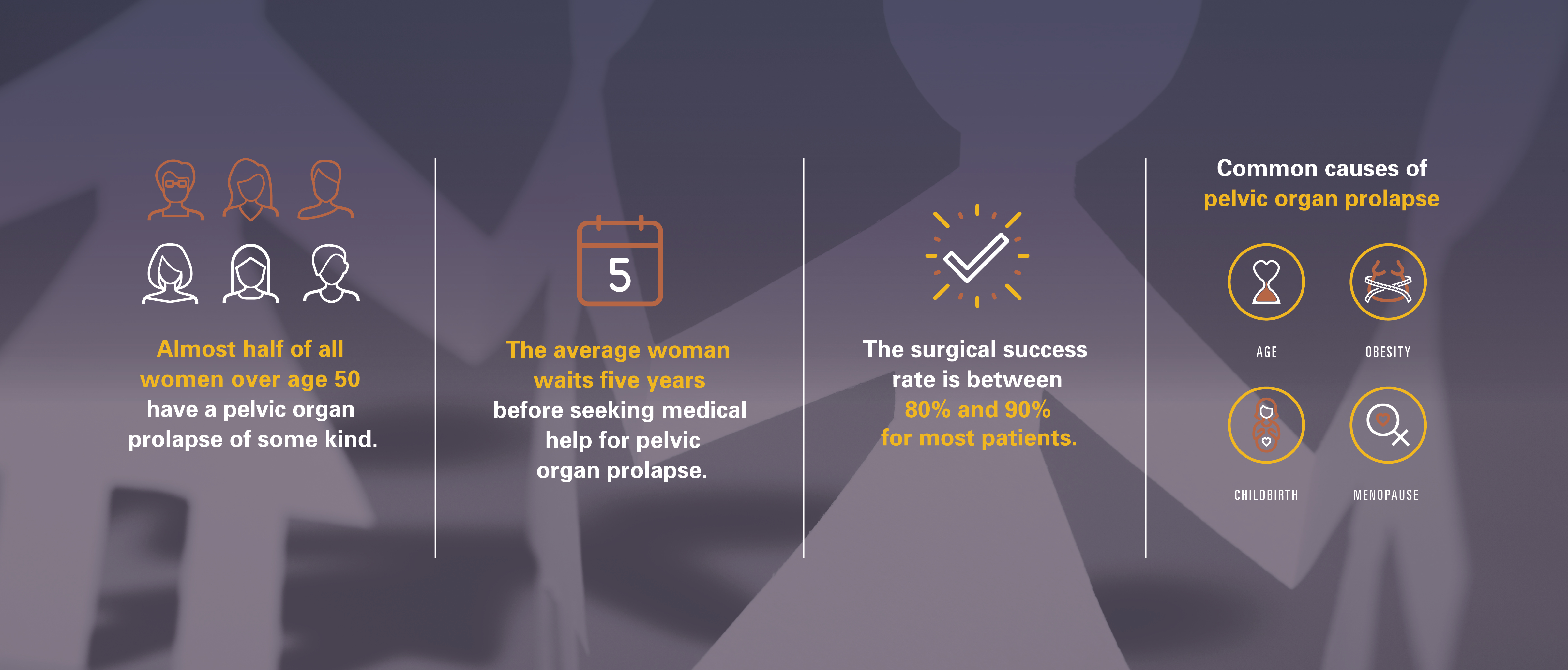
The average woman waits five years before seeking medical help for pelvic organ prolapse, often suffering silently as it infiltrates every aspect of her life. “Part of my delay in seeking treatment was that I was facing getting older,” adds Kim. “I felt like my body was failing me.”
Almost half of all women over age 50 have a pelvic organ prolapse of some kind. Prevalence increases with childbirth, which can injure surrounding muscles, and as a normal part of aging as estrogen levels decrease. Genetic and lifestyle factors—like smoking and obesity— can increase the risk of developing the disorder.
Mustering up her courage, Kim went to see her general practitioner, who encouraged her to schedule an appointment with a specialist. Walking in the parking garage, she saw a flyer for Gazala Siddiqui, MD, a urogynecologist at UT Physicians, the clinical practice of McGovern Medical School at UTHealth.
Once again, she pulled together her nerves, this time to visit the website on the flyer. After watching a video of Siddiqui, she immediately felt at ease.
“I thought, ‘I could trust this person,’ so I scheduled an appointment with her,” says Kim. “And when I met her at her office in Bellaire, I just fell in love with her—even though I didn’t like what she told me, which was that I needed surgery.”
“The success rate for most patients is around 80% to 90%,” explains Siddiqui. “There is no benefit in waiting—it’s about your quality of life.”
Yet even with the high success rate, Kim was uneasy about having surgery. “I had never had anesthesia before. So, that was an extra fear which was probably unfounded,” says Kim.
Siddiqui is quick to explain that treatment rests in the patient’s hands. “You get to say when you are ready,” says Siddiqui. “Seeing a doctor can help your symptoms from getting worse.” She adds that surgery is not the only option. Pelvic floor exercises and a pessary device, which helps support pelvic organs, may be the best option for mild prolapse.
“Dr. Siddiqui is a hidden gem. She’s extremely compassionate and caring about her patients,” says Kim. “She’s firm about what you need to do—but with good reason. She knows what is best for you and your recovery. And her staff was so friendly and helped normalize what I was going through.”
In Kim’s case, it was another 12 months before she felt ready to schedule her surgery at Memorial Hermann-Texas Medical Center. What surprised her was that there was virtually no pain after her surgery. The hardest part of her recovery was taking it easy for four to six weeks—no lifting heavy objects, no high-impact exercise. Her husband, Ken, stepped up to care for her during this time.
“I’m not used to people taking care of me; I’m extremely independent,” says Kim. “But my husband was a champ. It was really a nice time for us to be together.”
Her surgery was a success. After diligently following her post-op instructions, Kim was able to return to working nights as a nurse practitioner in the neonatal intensive care unit. She was able to golf and play with her grandchildren without discomfort or pain. And her relationship with her husband became even stronger.
“I wish I had done this years ago,” says Kim. “The quality of my life is so much better. I think about it pretty often, how much more comfortable I am in daily living.” Both Kim and Siddiqui encourage women experiencing symptoms not to wait. Break the silence.
“I think a lot of times, women don’t take care of themselves. As caretakers, everyone else comes first, and you go on the backburner,” adds Kim. “Taking care of myself was a big thing for me.”