Importance of emergency research
According to the Centers for Disease Control (CDC), there were 130.4 million visits to the emergency department in 2013 of which 32.2 million were injury-related visits. In 2014, injuries accounted for more than half the deaths in people younger than 45 years of age. In the United States, there were more than 192,900 deaths from injury, approximately one death every 3 minutes, was due to injury.1,2. There has been a focused effort to decrease the number of immediate deaths due to injury (speed limits, helmet laws, seat belts, to name a few). However, many people die after reaching the hospital due to hemorrhage or traumatic brain injury. There have not been enough rigorous research to study interventions to reduce the number of these kinds of death.
According to the CDC, heart disease is the leading cause of death in the United States. Each year in the United States, approximately 735,000 people have a heart attack. On average, every 42 seconds, someone in the United States has a heart attack.3 Stroke is the fourth leading cause of death in developed nations. Each year in the US, approximately 795,000 people experience a new or recurrent stroke. On average, every 40 seconds, someone in the United States has a stroke.4
One of the main difficulties in doing research in these emergency situations is that usually the patient is not able to give informed consent to take part in research studies. In most situations there are no family members who are available to give consent on behalf of the patient. Because of ethical concerns involved in doing research in a situation where the patients cannot give consent to take part in the research, a lot of widely accepted treatment that is given to patients in emergency settings have not been tested in rigorous clinical trials.
The United States Food and Drug Administration (FDA) has issued special regulations for doing research in emergency situation. The purpose of these regulations to allow certain kinds of emergency research trials to be done. According to FDA4, emergency research will help:
- Provide individuals in life-threatening situations access to potentially life-saving therapies;
- Advance knowledge through collection of information about effectiveness and safety; and
- Improve therapies used in emergency medical situations that currently have poor clinical outcomes.
Importance of informed consent
Respect for persons is a basic ethical principle for conducting research in human beings. One of the main aspects of respect for persons is to make sure that researchers provide information about the research study and ask for people to volunteer to join the research study. This is called informed consent.
Informed consent is the process of learning the key facts about a research study before deciding whether or not to take part. It is also a continuing process throughout the study to give new information about the research to participants. To help someone decide whether or not to participate, the doctors and nurses involved in the trial explain the details of the study such as risks, benefits and what would happen to them when they are in the research study.
Rationale for exception from informed consent.
In many emergency situations, the people who are taking part in the research study are not able to give their informed consent due to their condition, for example, they could be in coma due to injury or stroke. If the research were only done in patients who were able to consent, these patients may have had a better chance for fully recovering because they were in a better condition that the sicker patients. So doctors would not know if the patient recovered because they were in a better condition or because of the new treatment. In most of these situations, it is not possible to get consent from people in advance as it might not be possible to identify who might end up in the emergency room needing the treatment that is being studied.
Introduction to concept of therapeutic window.
Many of the treatments given in an emergency situation have to be given very quickly. For example, a patient with a large acute ischemic stroke might be losing up to 2 million brain cells every minute. So any delay in treatment could result in poorer outcomes. It would not be in the patient’s best interest to delay treatment while trying to identify family members to provide informed consent for taking part in the research study.
Description of community consultation efforts.
Before a planned emergency research study is done at UTHealth, the researcher must inform the Houston community about the proposed study. This will include details including:
- Clarify that informed consent will not be obtained for most (or all) research participants,
- Explain why consent is not possible,
- Inform the communities about all relevant aspects of the proposed research:
- Risks of the intervention being studied,
- Benefits of the intervention being studied,
- Invite members of the community to reach out to the researchers for more information,
- Invite members of the community to give feedback about the research,
- Provide information about ways in which who do not wish to be part of these studies can make their preference known to the emergency departments where the research will be done.
For each proposed study, researchers will meet with community members at various meetings in community centers, churches, patient support groups etc. When the study has been completed, the researchers will share the results of the research with the community.
If you would like UTHealth researchers to come speak at your community meeting about planned emergency research or any type of research, please write to us at clinicaltrials@uth.tmc.edu .
Description of additional protections for planned emergency research.
All research studies done at UTHealth in which people participate are reviewed by a group of people called the Committee for the Protection of Human Subjects. For planned emergency research studies, this Committee will review the researchers proposal and make sure that all the necessary precautions are taken to minimize risks to participants.
Planned emergency research studies must also have an independent group of experts called the data and safety monitoring board to review the data that is collected during the study to make sure that the risk benefit ratio is favorable for the participants.
Opting out of emergency research that is done without informed consent.
If you do not wish to take part in a planned emergency research study done under ‘exception from informed consent’ at UTHealth, please contact clinicaltrials@uth.tmc.edu to obtain a bracelet and a card which you must carry at all times when the study is being conducted. We will keep you informed of all ongoing and upcoming studies done under ‘emergency exception from informed consent’ on this website.
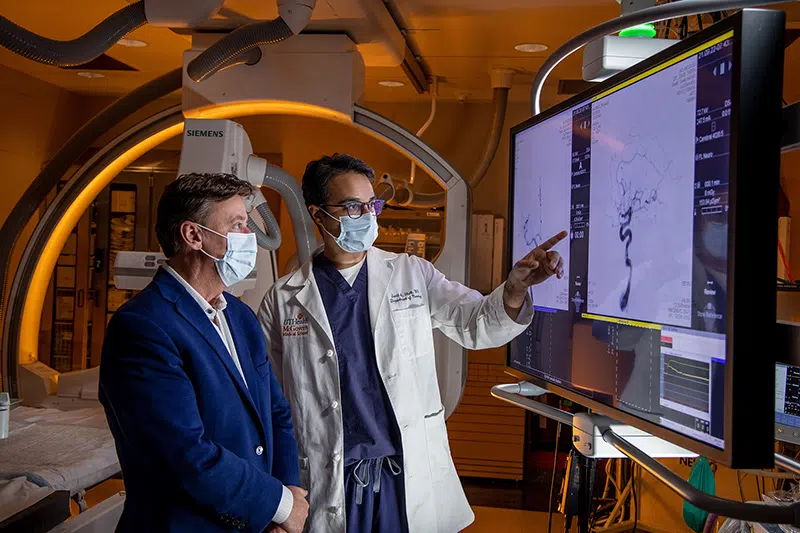
ONGOING TRIALS AT UTHEALTH INVOLVING EXCEPTION FROM INFORMED CONSENT
- TOWAR Trial
- CriSP-HS
- MATIC-2 (MATIC-2 Spanish)
More information on planned emergency research:
More information on randomization:
More information on informed consent:
References:
- CDC Key Injury and Violence Data
- National Center for Health Statistics
- CDC Heart Disease Facts
- CDC Stroke Facts
- FDA Planned Emergency Research